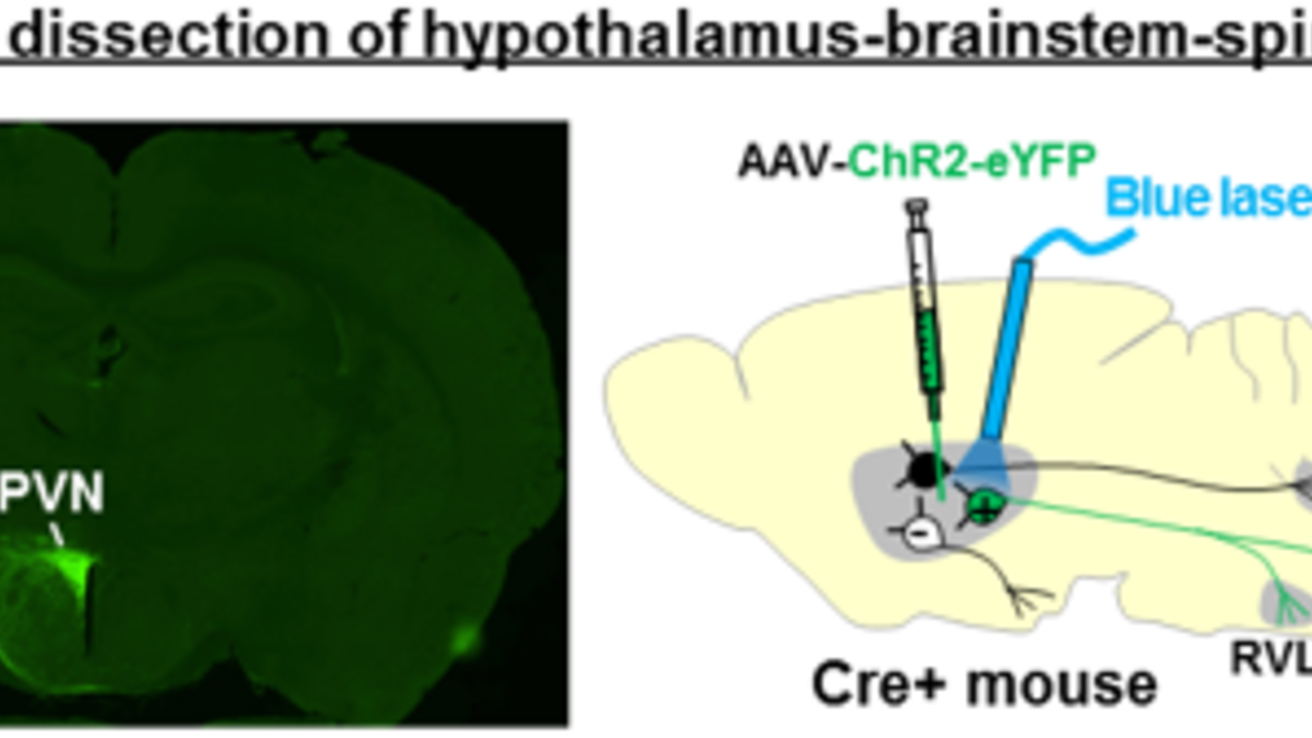
Hypothalamic-brainstem circuits in obesity and obesity-associated hypertension and sleep disorders
Hypothalamic and brainstem circuits are crucial for maintaining physiological homeostasis, including body weight, blood pressure, and sleep regulation. While leptin and melanocortin signaling appears to be critical for these physiological processes, underlying neural circuits remain incompletely understood. Using a variety of different transgenic mice and viral vectors combined with cutting edge neuroscience techniques, including optogenetics, chemogenetics, and fiber photometry, we aim to identify critical hypothalamic-brainstem circuits through which leptin and melanocortin signaling coordinately regulate these physiological processes. We hope the findings from this line of investigation will shed new light on underlying neurobiology of obesity and obesity-associated complications including hypertension and sleep disorders.
Neurobiology of eating disorders
Eating disorders, such as anorexia nervosa (AN) and bulimia nervosa (BN), are common and severe forms of mental illness characterized by marked disturbances in eating patterns, and have highest mortality rate of any psychiatric illness. While the neurobiological basis of eating disorder is incompletely understood, current theories highlight a combination of genetic and environmental factors that may disrupt neurotransmission in the brain networks affecting reward and social cognitive processes. Through family-based genetic linkage analysis combined with next generation sequencing, we have previously identified two rare missense mutations in the genes encoding estrogen-related receptor alpha (Esrra/ERRα) and histone deacetylase 4 (HDAC4) that are associated with increased susceptibility for AN and BN. Based on these human genetic findings, we have generated a variety of different transgenic mice that allow targeted manipulation of Esrra and HDAC4 in the brain and currently working on to gain deeper insights into the underlying neurobiology of eating disorders.
